Acute diverticulitis – CT
This CT was performed for a 60 year old woman who presented to ED with fever and left lower quadrant pain.
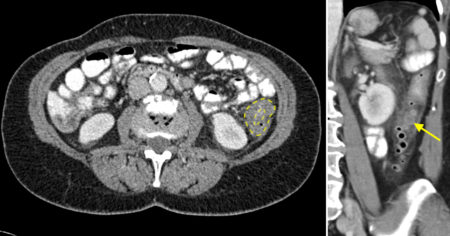
On the transverse image, left, there is marked thickening of the wall of the descending colon. The inner and outer margins of the wall are outlined by the yellow lines – the oedematous wall between these lines measures up to a centimetre. Compare this to the normal, almost-imperceptible wall in the other visualised small and large bowel segments elsewhere in the abdomen. The fat around this segment of colon is ill-defined, suggesting an inflammatory process.
The differential diagnosis for focal colonic wall thickening includes ischaemic colitis, infectious colitis, inflammatory bowel disease, diverticulitis and neoplasia.
In this case, the cause is very nicely demonstrated on the coronal image, right. There are multiple gas-filled diverticula, and in the midst of these there is a diverticulum that contains fluid (arrow). The inflammatory fat-stranding around the colon appears to be centred on this particular diverticulum. The findings are typical of acute diverticulitis.
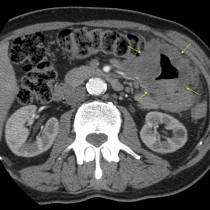
Having made this diagnosis CT, the radiologist must then search for the potential complications. Perforation and abscess formation are the most common of these; abscesses are usually located in the vicinity of the abnormal colon but occasionally will be found some distance away, sometimes in the liver. Most of these abscesses will be amenable to percutaneous drainage in Interventional Radiology.
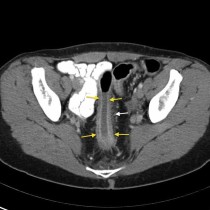
Less common complications include stricture formation with bowel obstruction, and the formation of a fistula (to another bowel segment or to the bladder or vagina). Fistulae to the bladder (colovesical fistulae) can often be predicted on CT by the presence of air (or even oral contrast) in the bladder lumen.