Giant cell arteritis
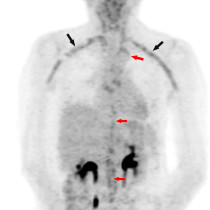
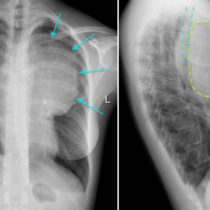
This was an interesting incidental finding on a PET/CT performed on a 78-year-old woman as part of her work up for a squamous cell carcinoma in her neck.
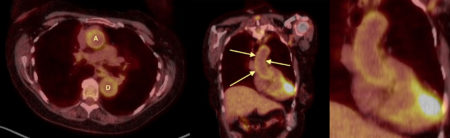
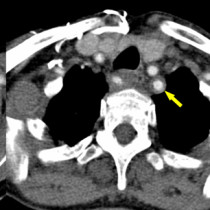
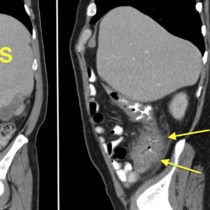
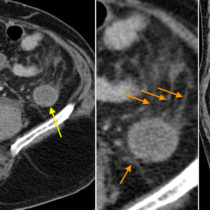
There is uniform, circumferential increased fluoro-deoxy-glucose (FDG) uptake in the walls of the ascending (‘A’) and descending (‘D’) thoracic aorta. This is particularly well seen in the ascending aorta on the coronal image (arrows, and magnified on the right-hand image).
The appearances are consistent with large vessel vasculitis; in a female patient of this age we would expect a diagnosis of giant cell arteritis (GCA) rather than Takayasu’s. A temporal artery biopsy was performed and confirmed GCA.
This case was unusual in that it was an incidental asymptomatic finding, but it illustrates an interesting point that medical students are often unaware of: PET/CT’s increasing role in the evaluation of inflammatory as well as neoplastic disease. PET/CT can be used for the initial diagnosis of vasculitis when alternative imaging techniques (and temporal artery biopsy) are negative or indeterminate, as well as for monitoring response to treatment and confirming suspected recurrence. It is also a useful imaging technique in the work-up/follow-up of other inflammatory processes, for example retroperitoneal fibrosis, and as a method of isolating the problem in patients with pyrexia of unknown origin (PUO). GCA will turn out to be the underlying diagnosis in around 1 in 6 cases of PUO1.
PET/CT has much higher sensitivity than other imaging modalities (temporal artery ultrasound, whole body CT angiography and MRI) for vasculitis, and it has a reported specificity of up to 100%1. The degree of FDG uptake within the artery walls has been shown to correlate very well with the degree of elevation of the patient’s inflammatory markers (ESR, CRP). It is, however, not as readily available and as a result priority for PET/CT slots still tends to be given to oncology patients.
Reference:
- Zerizer I, et al. Role of PET/CT in the diagnosis and management of vasculitis. Eur J Radiol 2010;73:504-509.