Shoulder dislocation with Bankart fracture
An important thing to look for when a post-reduction radiograph of the shoulder has been performed on someone who presented with a glenohumeral dislocation is an associated fracture. The two bony structures that are commonly injured when the humeral head dislocates are the anteroinferior rim of the glenoid and the posterosuperior aspect of the humeral head and greater tuberosity, as they strike each other during the injury. When the glenoid fractures, the injury is called a Bankart fracture; when the humeral head is injured it may result in an impaction fracture (with no displaced bone fragments, called a ‘Hill-Sach’s deformity’) or occasionally results in a displaced fracture of the greater tuberosity.
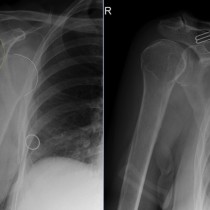
This case is a typical example of a Bankart fracture. The image on the left shows the dislocated humeral head – the yellow line indicates the rim of the glenoid, and the orange line outlines the humeral head which should normally be situated lateral to the yellow line. This is an anteroinferior dislocation, which is by far the most common type of shoulder dislocation. On the post-reduction image, right, we can now see a curved fragment of bone inferior to the joint (arrow), which represents the displaced fracture of the glenoid rim. It’s just about visible on the first image but would be easily overlooked.
Both Bankart fractures and Hill-Sach’s deformities can predispose to recurrent shoulder dislocation therefore many of these will subsequently require surgery to stabilise the joint.
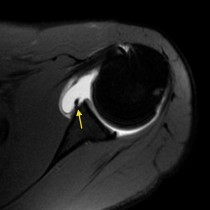
An additional injury that can occur during shoulder dislocation and result in recurrent instability is called a Bankart lesion (not a fracture), where instead of a fragment of bone breaking off the glenoid, instead the glenoid labrum is torn. Obviously this is not going to be visible on a radiograph. When a Bankart lesion is suspected, typically in someone who has recurrent dislocation, we are usually asked to performed an MR arthrogram of the shoulder. This involves injecting a dilute solution of MRI contrast (gadolinium) into the joint prior to the MRI, which makes it much more sensitive for picking up labral tears. There is a link to an example of this below.