Thoracic aortic dissection – CT
This 80-year-old man presented to the ED with acute onset of chest pain.
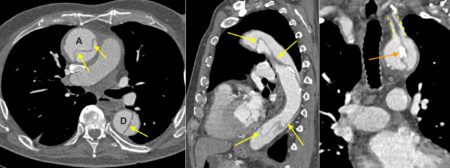
His arterial phase CT shows the typical features of a Stanford type A dissection of the thoracic aorta. The left-hand transverse image shows the dissection flap (arrows) extending through the ascending (‘A’) and descending (‘D’) aorta. The flap is shown more clearly on the middle, sagittal image. On the right, the coronal CT image shows the dissection flap extending into the left common carotid artery, which is outlined by the dashed yellow line.
As you will remember, aortic dissection is stratified into one of two classifications based on the requirement for surgical intervention. Stanford type A dissections involve the ascending thoracic aorta, account for the majority of cases and have a high mortality rate if not treated with emergency surgery1. Stanford type B dissections involve the descending thoracic aorta, distal to the origin of the left subclavian artery. These are typically treated medically with management of hypertension, however some cases may require treatment by surgery or interventional radiology if complications , such as aortic rupture or end-organ ischaemia, develop.
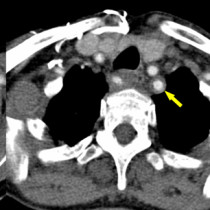
While CT is the modality of choice in patients with suspected dissection, a CXR is often performed initially. This may show a widened mediastinum. If the dissection has ruptured into the pericardium, massive cardiomegaly may be evident. Similarly, rupture into the left pleural space may occur resulting in a pleural effusion. Another potential radiographic sign to look for is displacement of calcification of the aortic wall – this is a subtle finding that is easier to spot if we have a previous CXR for comparison. In the example shown here, the right-hand image shows a nice example of displaced calcification (orange arrow), which has moved into the centre of the aorta with the intimal flap.
On CT, the intimal flap is visible in the majority of cases, dividing the aorta into a true lumen and a false lumen. In addition to permitting us to correctly diagnose and classify aortic dissection, CT also allows us to identify the potential complications of dissection which include pericardial tamponade or aortic rupture into the pericardium, pleural space or mediastinum. We also use CT to assess for occlusion of aortic branches due to the dissection – for example, the carotid, subclavian, renal or mesenteric arteries may be occluded. For this reason, when thoracic aortic dissection is suspected, we routinely extend the CT as far as the pelvis to ensure that all of the aortic branches are included.
Reference:
- McMahon M et al. Multidetector CT of aortic dissection: a pictorial review. Radiographics 2010;30:445-60. DOI: http://dx.doi.org/10.1148/rg.302095104